Glaucoma tube-shunt implants
Glaucoma tube-shunt implant surgery is a complex glaucoma procedure that is normally reserved for patients with refractory glaucoma and uncontrolled eye pressures even on maximum glaucoma medications, and also when conventional glaucoma filtration surgery (trabeculectomy) is unlikely to be successful. This is either due to the complexity of the eye conditions or the eyes have high risk of scarring response that would make other types of glaucoma surgeries unlikely to be successful.
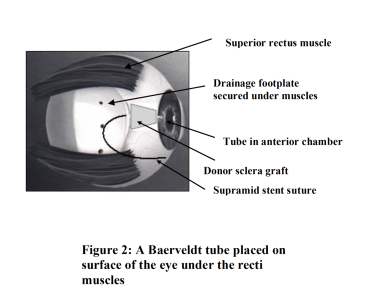
The tube shunt (figure 1) is a silicon tube measuring about 0.5 mm diameter. One end of the tube is inserted into the eye (anterior chamber) and the other end is connected to a silicon plate resting on the surface (sclera) of the eye behind the eye lids, it is acting like a reservoir for the water (aqueous) from inside the eye to be drained away in order to maintain a normal eye pressure.
Figure 2: A schematic diagram of a Baerveldt tube positioned under the superior and inferior recti muscles. The tube portion is covered by a donor sclera graft. The tube is inserted inside the eye (anterior chamber). The whole structure is covered by the upper eye lid, so there is very little change to the external appearance of the eye after the operation.
What are the benefits?
The benefits of this surgery are to improve the eye pressure control and preserve the remaining vision. This operation is unlikely to improve vision.
The tube shunt operation is generally a very successful operation for refractory glaucoma. The success rate is about 85% in 3 years and 70% in 5 years in terms of successfully controlling the eye pressure. However, some patients may need to return to use glaucoma eye drops to maintain a satisfactory eye pressure level.
What are the risks?
The common risk of this operation is temporary low eye pressure that can happen when the tube-shunt starts working at 6-7 weeks after the operation. If the eye pressure becomes too low, an injection of some ‘jelly like’ substance (viscoelastics) into the eye may be necessary to maintain the eye pressure until it is stabilised. This procedure is usually done in the out-patient.
Other risks of the operation including infection, bleeding inside the eye, corneal decompensation (cloudiness at the front surface of the eye), and very rarely loss of vision.
What are the risks of not having the operation?
The risks of uncontrolled raised eye pressure are continuing damage to the optic nerve and subsequent gradual loss of vision and eventual blindness.
Raised eye pressure can also cause pain and blockage of blood vessels on the retina.
Are there any alternatives to this operation?
The alternatives of this operation are other types of glaucoma surgeries e.g. laser (cyclodiode) procedure or conventional trabeculectomy. But the tube-shunt implant operation is only offered when other procedures are unlikely to be successful in controlling the eye pressure for a long period of time.
Preparing for the operation.
The operation is normally carried out under general anaesthesia. Patients will need to attend a pre-operative assessment before surgery for assessment of their general health, medications and fitness for general anaesthesia. Patients will need to be nil by mouth for at least 6 hours prior to the surgery.
If patients are on warfarin tablets, they will require blood test within one week before surgery to make sure the clotting level is suitable for the surgery to avoid excessive bleeding during operation.
Some patients on the new types of anti-clotting tablets may require stopping before surgery, this will be assessed at the pre-assessment clinic and instructions will be given to the patients.
During the operation.
The procedure will be carried out under general anaesthesia. When patients arrive to the operating theatre, the anaesthetist will insert a tiny needle on the back of the hand and leave a tiny plastic tube in there for administration of the general anaesthesia. Patients will slowly drift to sleep after injection of the anaesthetic medicine. The anaesthetists will look after the patients throughout the whole operation. The procedure will normally take at least 2 hours to perform.
When the operation is completed, the patients will wake up at the recovery area of the theatre. Patients will have an eye pad and plastic shield covering the operated eye. Patients may experience some discomfort with the eye but not severe pain.
After the operation
Patients will be moved back to the eye ward. If there is excessive pain, patients can request pain killer tablets. However, this is rather rare that patients will require pain killer after the operation as a long-acting local anaesthetic injection is normally injected under the eye ball at the end of surgery. Therefore, most patients are quite comfortable after the surgery.
Some patients may require staying on the ward overnight after the surgery especially for patients travelling from far away. But most patients can go home on the same day after surgery and return the next day for post-operative checks.
Going home
It is advisable that patients should have someone accompany them to go home. Patients will be given the discharge medications including eye drops and tablets for use after the operation.
The eye pad covering the operated eye will need to stay until the next morning when it can be removed by removing the adhesive tapes over the eye pad. Patient may see some dry blood on the eye pad after removal, but no bleeding is expected after removal of the eye pad. If there is any active bleeding from the eye, patients should replace the eye pad and return to the eye hospital immediately for assessment.
Patients are usually required to return to clinic for assessment the morning after the operation. Apart from the routine post-operative medications, patients will be advised on the use of glaucoma medications at the first day assessment. Patients are normally required to return for review at 1 week, 3 weeks and 6 weeks after surgery.
We generally advise patients to stop going to school or work for about 2 weeks after surgery. Patients should avoid driving in the first week if the other eye has normal eye sight. If the operated eye is the only eye with good eye sight, then patients must stop driving until the eye sight has return to the level that is legally safe to drive. Patients should refine from vigorous exercise until the eye pressure is stabilised in 2 months, but gentle exercise and normal daily activities are not restricted.
Follow-up
The tube-shunt will start to work at 6-7 weeks after surgery, the eye pressure may suddenly dropped to a very low level that require intervention Therefore, it is very important for patient to return to clinic for assessment during this period to ensure the tube-shunt has commenced to work and the eye pressure is maintained to a normal level. If the eye pressure is too low<5mmHg, we may give an injection of a jelly substance inside the eye in the clinic to increase the eye pressure and prevent problems from low eye pressure. Some patients may require weekly visit until the eye pressure becomes stabilised.
The post-operative steroid eye drops are normally tapered off over a 3 month period and the oral steroid is to be tapered over a 3 weeks period. Most patients are required to continue the glaucoma eye drops until the tube starts working in 6-7 weeks’ time.
Symptoms to report
Patients should few fairly comfortable after surgery but the vision can be rather blurred. But if there is severe pain or loss of vision, patients need to return to the eye casualty department at Birmingham and Midland Eye Centre for emergency consultation.
If patients experience severe discomfort after putting the eye drops in, patients may be developing an allergic reaction to the eye drops. Patients should contact us for earlier assessment that may require a change of the post-operative treatments.